Benign prostatic hyperplasia (BPH), also known as lower urinary tract symptoms (LUTS), is a common urological condition caused by the non-cancerous enlargement of the prostate gland in aging men. As the prostate enlarges it squeezes down on the urethra causing men to have trouble or difficulty with urinating. Risk factors for developing BPH include increasing age and a family history of BPH.
Benign prostatic hyperplasia (BPH), also called benign prostatic hypertrophy, is not simply a case of too many prostate cells. Prostate growth involves hormones, occurs in different types of tissue (e.g., muscular, glandular), and affects men differently. As a result of these differences, treatment varies in each case. There is no cure for BPH and once prostate growth starts, it often continues, unless medical therapy is started.
The prostate grows in two different ways. In one type of growth, cells multiply around the urethra and squeeze it; much like you can squeeze a straw. The second type of growth is middle-lobe prostate growth in which cells grow into the urethra and the bladder outlet area. This type of prostate growth typically requires surgery.
BPH is a very common condition with aging men and it will affect approximately 50 percent of men between the ages of 51 and 60 and up to 90 percent of men over the age of 80.
Benign Prostatic Hyperplasia Signs & Symptoms
Since the prostate surrounds the urethra just below the bladder, its enlargement can result in symptoms that irritate or obstruct the bladder. The most common symptom is frequent urination (as often as every 2 hours) especially at night. Other symptoms include the sensation that the bladder is not empty even after urination or the inability to hold urine once the urge to urinate arises. BPH can cause a weak urinary stream, dribbling of urine, or the need to stop and start urinating several times when the bladder is emptied. BPH can cause trouble in starting to urinate, often requiring a man to push or strain in order to urinate. In extreme cases when a man is no able to urinate because of a significantly enlarged prostate can require emergency catheterization to empty the bladder.
A man should see a doctor if he has any of the symptoms mentioned previously that are bothersome. In addition, he should see a doctor immediately if he has blood in the urine, pain with urination, burning with urination or is unable to urinate.
Benign Prostatic Hyperplasia Diagnosis
In order to help assess the severity of such symptoms, the American Urological Association (AUA) BPH Symptom Score Index was developed. This diagnostic system includes a series of questions that ask how often the urinary symptoms identified above occur. Please take the test on our site to learn your score.
When a doctor evaluates someone for possible BPH, the evaluation will typically consist of a thorough medical history, a physical examination (including a digital rectal examination of the prostate or DRE), and use of the AUA BPH Symptom Score Index. In addition, the doctor will generally do a urine test called a urinalysis. There are a series of other studies that may or may not be offered to a patient being evaluated for BPH depending on the clinical situation:
- a measurement of post-void residual volume (PVR), the amount of urine left in the bladder after fully emptying the bladder
- uroflowmetry, or urine flow study, a measure of how fast urine flows when a man urinates
- cystoscopy, a direct look in the urethra and/or bladder using a small flexible scope
- urodynamic pressure-flow study that tests the pressures inside the bladder during urination
- ultrasound of the kidney or the prostate
- prostate specific antigen (PSA), a blood test to screen for prostate cancer
- urinary cytology, a urine test to screen for bladder cancer
Benign Prostatic Hyperplasia Treatment
If you are diagnosed with BPH, you should discuss all treatment options with your urologist. Together, you can decide whether medication, minimally invasive therapy or surgical treatment is best for you. There are multiple medications and surgical procedures that are available to treat BPH and having a complete open conversation with your urologist will help you better decide which option is best for you. We have listed a few surgical treatments below.
UroLift
The UroLift® System Treatment
What is the UroLift System?
Treatment with the UroLift® System uses a minimally invasive approach that provides rapid relief and recovery of BPH symptoms.1 It is an earlier treatment option that can get men off BPH medications and avoid major surgery. The goal of the UroLift System treatment is to relieve symptoms so you can get back to your life and resume your daily activities.
The UroLift® System treatment has demonstrated a significant improvement in quality of life for patients that is greater than reported for medications.2,3 The UroLift® System is the only BPH procedure shown not to cause new and lasting erectile or ejaculatory dysfunction*, while being a safe and effective treatment of lower urinary tract symptoms due to BPH.1,3-6
How Does The UroLift® System Work?
The UroLift® System uses a revolutionary approach to treating BPH that lifts and holds the enlarged prostate tissue so it no longer blocks the urethra. It is the only available BPH treatment performed by a urologist that does not require heating, cutting, or removal of the prostate tissue. The procedure is typically performed using local anesthesia in a physician’s office or ambulatory surgery center. Patients typically return home the same day without a catheter.1
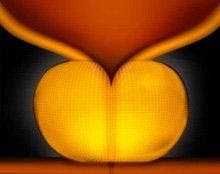
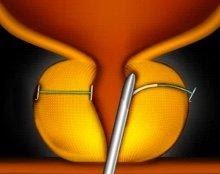
Enlarged Prostate
An enlarged prostate can narrow or even block the urethra, causing bothersome urinary symptoms.
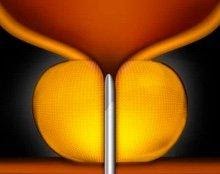
Step 1
The UroLift Delivery Device is placed through the obstructed urethra to access the enlarged prostate.
Step 2
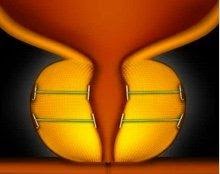
Small UroLift Implants are permanently placed to lift and hold the enlarged prostate tissue out of the way and increase the opening of the urethra.
Step 3
The UroLift Delivery Device is removed, leaving an open urethra designed to provide symptom relief.
1. Roehrborn, J Urol 2013, L.I.F.T. Study
2. AUA Guidelines 2003
3. Roehrborn et al. Can J Urol 2017
4. Roehrborn, Can J Urol 2015, 3-Year L.I.F.T. Study
5. Roehrborn, Urology Practice 2015, 2-Year L.I.F.T. Study
6. Roehrborn Urology Clinics 2016
*No instances of new, sustained erectile or ejaculatory dysfunction
Frequently Asked Questions
Who is a good candidate for the UroLift® System treatment?
You may be a good candidate if you are a male, 45 years of age or older, and have symptoms relating to BPH. Speak with your urologist to see if the UroLift® System treatment is right for you. If you have a known allergy to nickel, titanium or stainless steel, talk to your doctor about your allergy before getting a UroLift System treatment.
What should I expect during the treatment? Is it painful? How long does it take?
If you and your doctor decide that the UroLift® System treatment is right for you, your doctor will provide you with more detailed information relating to the treatment. In general, the UroLift System is a minimally invasive treatment that entails minimal downtime. Your doctor will use the UroLift Delivery Device to deploy permanent implants to relieve obstruction caused by the enlarged prostate that is pressing on your urethra. The procedure, which usually takes about an hour, may be performed under local or general anesthesia and you may be given medication to feel comfortable during treatment. This typically helps minimize discomfort during the procedure, though everyone’s definition for pain and discomfort varies greatly. Typically, no catheter and no overnight stay is required post-treatment.1
What happens post-treatment, during the recovery period? Are meds required?
After the treatment, patients typically go home the same day without a catheter. There is minimal downtime post treatment and many patients experience symptom relief in as early as 2 weeks. Patients may experience some urinary discomfort during the recovery period. Most common side effects are mild to moderate and include pain or burning with urination, blood in the urine, pelvic pain, urgent need to urinate and/or the inability to control the urge. Most symptoms resolved within two to four weeks after the procedure.
Does the treatment affect my sexual function?
Clinical studies have shown the UroLift® System treatment does not cause new, sustained instances of erectile or ejaculatory dysfunction.1 The same cannot always be said of other BPH therapies such as TURP, laser, and even medication.1-4
Does my insurance cover the treatment?
The UroLift® System treatment is covered by Medicare and all major private insurers. Contact your insurance provider for your specific coverage information.
1. Roehrborn, J Urology 2013 LIFT Study
2. AUA BPH Guidelines 2003, 2010, 2018
3. Naspro, Eur Urol 2009
4. Montorsi, J Urol 2008
Talking to Your Doctor about BPH
BPH is a very common condition and is one of the leading reasons men visit a urologist. Whether you have just started experiencing symptoms or if you’ve tried various medications or even surgery, there are a range of treatment options available.
Before you visit the doctor’s office, you can take this BPH Symptom Quiz, designed by the American Urological Association, to determine the severity of your symptoms. We will discuss your symptoms together to decide which treatment option is best for you.
Schedule an appointment today to discuss your BPH symptoms with us.
Photoselective Vaporization of the Prostate (PVP)
Photoselective vaporization of the prostate (PVP) is a minimally invasive procedure that uses a special high-energy laser (e.g., GreenLight PVP™ Laser) to vaporize excess prostate tissue and seal the treated area. The procedure is performed on an outpatient basis in a hospital or surgical center and may be performed under local, spinal, or general anesthesia. PVP takes between 10 and 30 minutes to perform, depending on the size of the prostate and patients are usually discharged within a few hours.
The type of laser used in PVP is delivered to the prostate through an endoscope (device that consists of a tube and an optical system) that is inserted into the urethra. The procedure prevents damage to surrounding tissue and minimizes side effects such as pain, blood in the urine (hematuria), and swelling.
Many patients do not require a catheter after PVP, and those who do typically are catheterized for less than 24 hours. Patients are advised to avoid strenuous exercise for 2 weeks following the procedure and can usually resume regular activities the next day. PVP provides immediate and long-lasting results comparable with other minimally invasive procedures.
Transurethral Vaporization of the Prostate (TUVP)
Transurethral vaporization of the prostate (TUVP), also called vaportrode, involves direct application of heat (under 100° F) to the prostate tissue with a grooved roller-bar that vaporizes tissue. The immediate tissue loss leads to quick improvement of symptoms. The procedure takes from 20 to 65 minutes. The catheter is usually removed within 24 hours and most patients go home within 2 days.